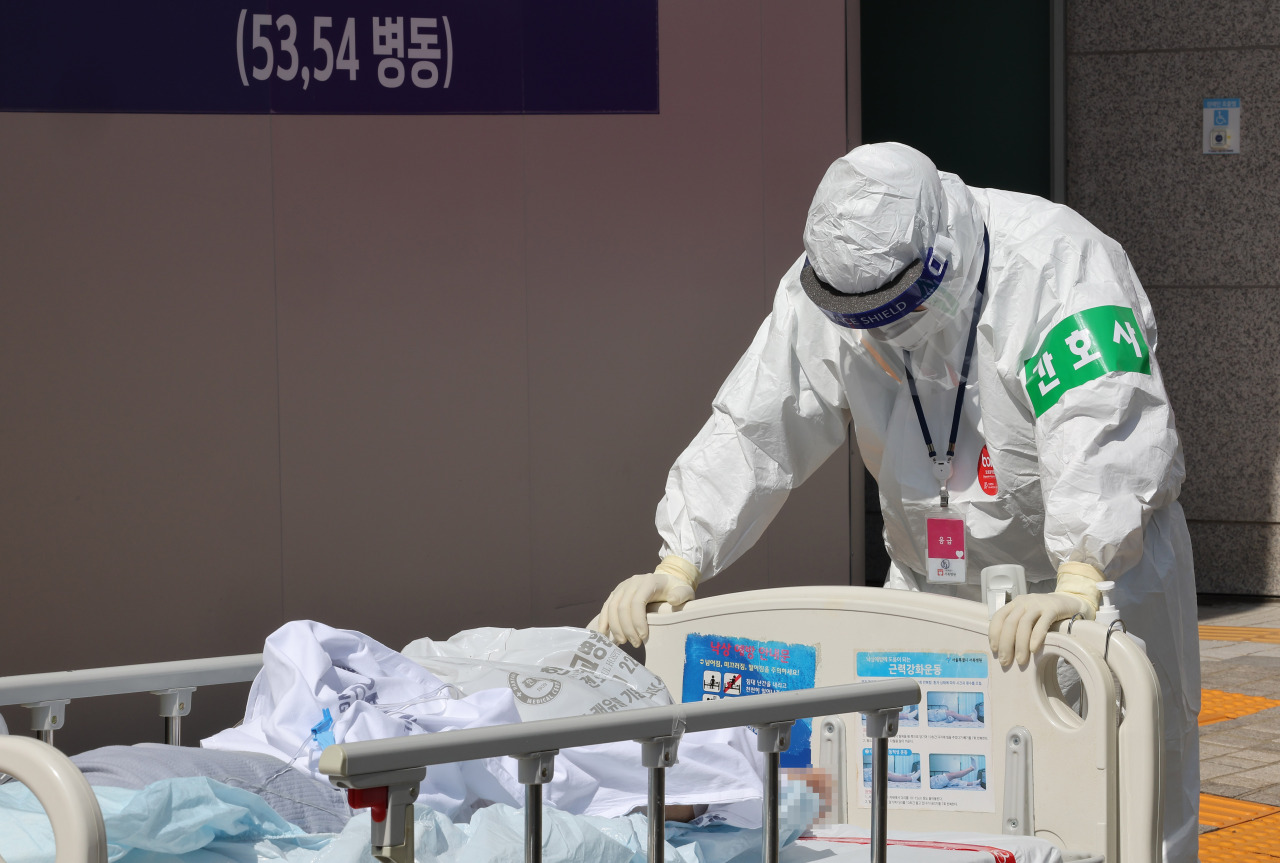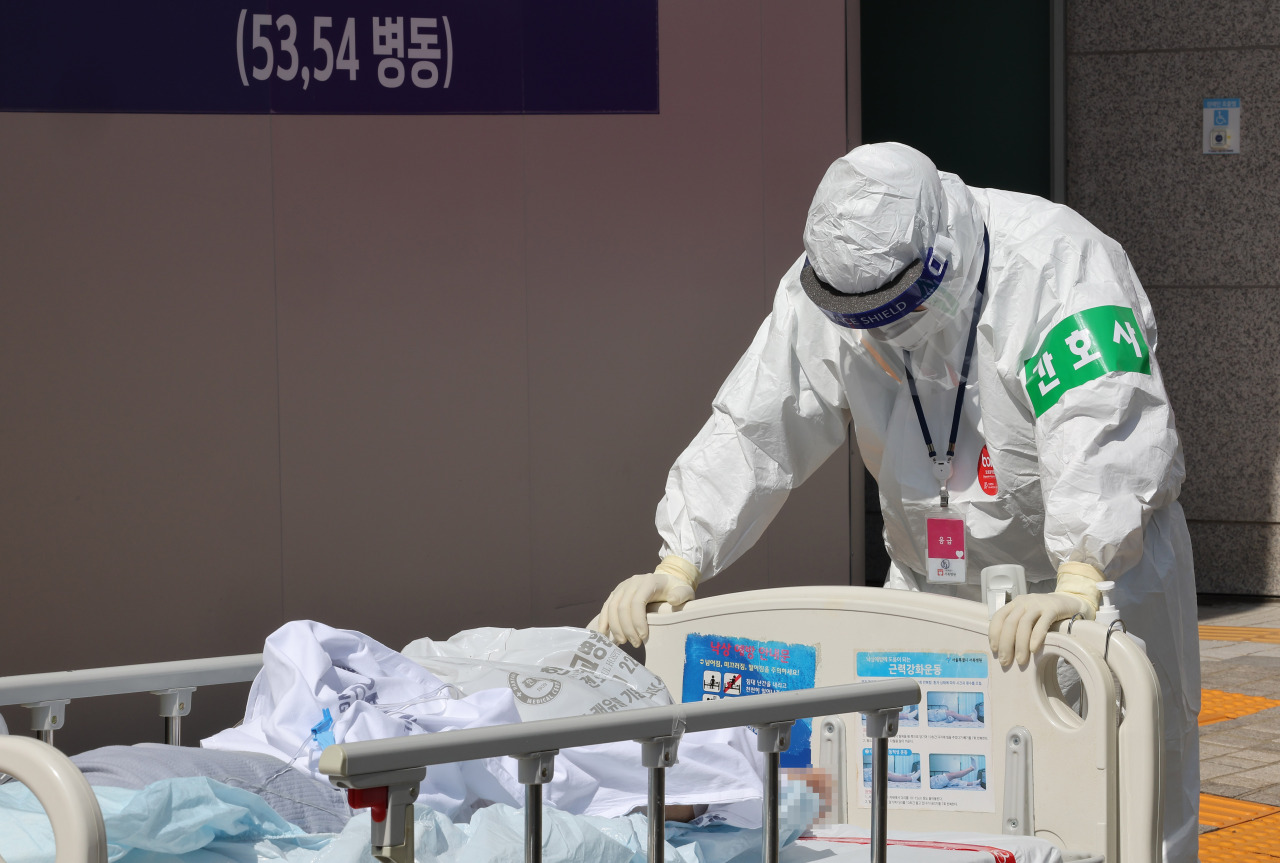
A nurse in a protective suit transfers a COVID-19 patient on Tuesday at a hospital in Eunpyeong, a northern Seoul district. (Yonhap)
COVID-19 patients who remain sick beyond the seven-day isolation are struggling to find access to care and pay hospital bills.
In January, as omicron’s share of new cases was rising, the government shortened the isolation period to seven days. Once the seven-day isolation expires, all COVID-19-related medical costs are no longer covered by the government.
“The government considers a patient to no longer be a COVID-19 case past day seven. And yet some patients are still on oxygen therapy and other invasive procedures like extracorporeal membrane oxygenation, or ECMO, due to health damages from COVID-19,” families of survivors said in a joint statement on March 23.
In the statement they said patients were forced to give up their spot in intensive care units before they had fully recovered. In late December the government first introduced guidelines dictating the maximum length of stay at ICUs in order to speed up turnover amid bed shortages.
The legally required isolation period was like “a minimum time allowed to patients for ensuring that they get care,” they said, and it ignored the reality of many patients with severe symptoms who are unable to recover in a week.
On this the Ministry of Health and Welfare’s spokesperson Son Young-rae told March 22’s press briefing that around three-quarters of severe or critical cases was due to underlying diseases rather than COVID-19 itself. He said on March 17 that half of COVID-19 fatalities were from preexisting health conditions.
The daughter of a patient who has been hospitalized for nearly three months after contracting COVID-19 said in the statement that her family was being charged about 5 million won ($4,100) a week, with the sum now totaling nearly 40 million won. All of those bills were the family’s responsibility.
She said she was now being told that her mother, despite being put on ECMO, needed to move out because she has “recovered from COVID-19.”
She said her mother, who was already frail before COVID-19 and in her 70s, was not immediately assigned a bed when her oxygen levels began to fall while she was isolating at home. Despite repeated requests she was told to wait. She believes that if her mother had gotten care in time, she would not have fallen sick so badly.
“I don’t understand why the government refuses to acknowledge my mother as a COVID-19 victim. She is in the ICU battling for her life because of COVID-19,” she said.
Under the same principle some municipalities have stopped providing funeral assistance to COVID-19 patients who die after the seven-day isolation. But statistics show the average time from diagnosis to death is much longer, at 15 to 17 days.
Seeking post-isolation care is also a challenge for patients who are less severely sick. Patients can reach telehealth services while they are still in isolation, but not afterward. Some hospitals and clinics are discouraging patients from seeking in-person visits immediately after getting out of isolation over concerns they may still be infectious.
This is posing a hurdle for those who still experience lingering symptoms. Known as post-COVID-19 syndrome, effects of the disease sometimes can last beyond four weeks since symptoms first appeared.
Dr. Choi Hongjo, a preventive medicine professor at Konyang University, pointed out that “our policies and discussions around them have centered on reducing the administrative burden, rather than on protecting patients.”
As a result of the policy, low-income patients and families in particular may decide not to continue treatment because of the financial burden, he warned.
While the omicron surge is still in full swing, Korea is preparing to dial down the medical response to COVID-19 to how it was before the pandemic, according to the latest announcements from the government.
Prime Minister Kim Boo-kyum said on March 17 that discussions were underway for downgrading COVID-19’s threat status so that hospitals can treat infected patients without having to isolate them. This move would clear the government of the responsibility to cover expenses for tests and treatments.
The no-cost policy for getting a COVID-19 test ended in Korea in January. Before rapid antigen test results were recognized as a diagnosis on March 14, polymerase chain reaction or PCR tests would cost patients under 60 years of age as much as around 100,000 won. The rapid antigen tests are much cheaper at around 5,000 won.
The unaffordable costs of COVID-19 hospitalization highlight the limit of Korea’s National Health Insurance Service, according to Dr. Kim Chang-yup, a Seoul National University professor of public health sciences and director of the People’s Health Institute.
He said the end of waivers under the state health insurance program was only “a matter of when,” as keeping it would mean patients of other diseases may face reduced coverage.
“However, funding for infectious diseases like COVID-19 should instead be taken up in a separate budget bill,” he said.
South Korea reported 347,513 cases and 237 deaths for the 24 hours of Monday. In the past week the country saw an average of 348,952 cases and 353 deaths a day, translating to a weekly case fatality rate of 0.1 percent. Roughly 68 percent of all ICU beds nationwide were occupied.
By Kim Arin (
arin@heraldcorp.com)